Issue 28, January 2007
Keep Clear of Malpractice When Providing Veneers!
Dear Fellow Bondodontists,
Wow, another year flew by. We must be having fun!! I think Mary and I continue to live in the fast lane.
2007 will be another great year for our programs. The Tahoe seminar on June 9 will feature Prof. Edward Lynch from Queen's University in Belfast. He in the inventor of the ozone therapy marketed by KaVo as Healozone. Many of you have heard me speak briefly on the topic in the last 3 years; here is the source of the best and most complete information. Eddie is also an expert on caries and its prevention so I asked him to present a summary of current concepts, what works and what does not. It is beginning to look like caries risk assessment and management may become the "standard of care" to preclude malpractice litigation. There are some commercially driven products but let's get the straight scoop from an expert. If you have a cervical sensitivity, perhaps Eddie or I can treat it on the spot. It only takes about 10 seconds and I have never missed! I will be presenting some selected restorative topics that supplement Eddie's presentation.
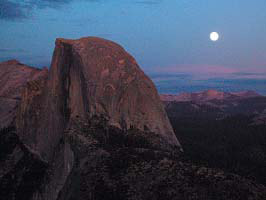
The Yosemite program on November 1-4 will feature Prof. Harald Heymann, one of our most popular speakers. He will be speaking on multiple restorative dentistry topics, among them: Insights into Abfractions and Desensitization, Direct Restoratives: Proven Solutions to Clinical Problems, Tooth Whitening: The Great White Hype! Harald strikes a prefect balance between science and practicality. The seminar is held at the Ahwahnee Hotel where Mary negotiated some very good room rates, not generally available to the public. The early November dates have proven to be excellent times for visiting Yosemite. This year the Glacier Point road was open and the views simply spectacular. A Glacier Point photo courtesy of our guest speaker, Dr. Ron Jackson:
Wow, another year flew by. We must be having fun!! I think Mary and I continue to live in the fast lane.
2007 will be another great year for our programs. The Tahoe seminar on June 9 will feature Prof. Edward Lynch from Queen's University in Belfast. He in the inventor of the ozone therapy marketed by KaVo as Healozone. Many of you have heard me speak briefly on the topic in the last 3 years; here is the source of the best and most complete information. Eddie is also an expert on caries and its prevention so I asked him to present a summary of current concepts, what works and what does not. It is beginning to look like caries risk assessment and management may become the "standard of care" to preclude malpractice litigation. There are some commercially driven products but let's get the straight scoop from an expert. If you have a cervical sensitivity, perhaps Eddie or I can treat it on the spot. It only takes about 10 seconds and I have never missed! I will be presenting some selected restorative topics that supplement Eddie's presentation.
The Yosemite program on November 1-4 will feature Prof. Harald Heymann, one of our most popular speakers. He will be speaking on multiple restorative dentistry topics, among them: Insights into Abfractions and Desensitization, Direct Restoratives: Proven Solutions to Clinical Problems, Tooth Whitening: The Great White Hype! Harald strikes a prefect balance between science and practicality. The seminar is held at the Ahwahnee Hotel where Mary negotiated some very good room rates, not generally available to the public. The early November dates have proven to be excellent times for visiting Yosemite. This year the Glacier Point road was open and the views simply spectacular. A Glacier Point photo courtesy of our guest speaker, Dr. Ron Jackson:
The penguin picture was taken on recent scouting trip, previewing a planned Antarctic cruise. If you are interested, let us know so that we can give you advance notice. We have a great Alaska cruise (sorry, no penguins there) scheduled for July 27. The cruise features a special guest speaker, Dr. David Winkler from London, one of Europe's finest clinicians. New Zealand is scheduled this year too. (New Zealand does have a few penguins.) It's Christchurch for June 29, Wellington July 4 and Auckland for July 7. There are usually some great airfare deals (especially the fly/drive deals) at that time of year. Winters in New Zealand are generally mild and a nice time to be there.
Have a great 2007.
Sincerely,
Ray Bertolotti
Have a great 2007.
Sincerely,
Ray Bertolotti
Keep Clear of Malpractice When Providing Veneers!
In 2005-2006, I was an expert witness in several malpractice lawsuits involving veneers. Clinical success should be sufficient to keep you out of trouble but unfortunately nothing is 100% successful, so be cautious. I offer the following opinions on how to avoid such litigation. Basically, it is by proper informed consent. Here is a slide I have been using recently as part of my Bondodontics 2006 presentation. I will discuss each issue below.
Some of the attorneys I have worked with recommend even more extensive informed consent such as for complications of anesthesia and even tooth loss. I personally think these are so unlikely that I don't generally include them, any more than I would with routine operative dentistry. Of course I'm not an attorney, so you might wish to consult your own attorney about this matter.
Permanent:
Amazingly, a frequent problem that leads to litigation is that patients somehow think veneers are"permanent". Now just what in restorative dentistry is permanent? I can only think of extraction. So let's be sure to inform about expected longevity and especially what happens when they do need replacement. Now think about how advantageous it would be to replace veneers that are entirely in enamel, compared to those placed on heavily prepped teeth, well into dentin. If you don't know the procedure for conservative veneers, may I humbly suggest that you attend my seminar? I also recommend Ross Nash Seminars for such. (If you can't make it to a seminar, one top reference is: Fracture load and mode of failure of ceramic veneers with different preparations. Castelnuevo et al, J Pros Dent 2000;83:171-180).
Irreversible:
DenMat has been advocating "no prep" (reversible) veneers since the 1980's. Lately they seem to have revived the concept with some heavy promotion which has led to increased public and dentist awareness. They seem to have mastered the process of producing very thin veneers. Of course DenMat can work well with prepped teeth too. On most well aligned teeth, I prefer conservative in-enamel preparations for enhanced esthetics and potentially better periodontal response. I tell most of my patients about the advantages I perceive of conservative (in enamel) tooth reduction but of course also the trade-offs compared to "no prep" veneers. My occasional "no-prep" veneers are mostly done on lingually tipped incisors or on peg-shaped lateral incisors. If you do prep, especially heavily and that often means into dentin, be sure that your patients understand. They should be told that occasionally a crown (and perhaps endo too, to be safe) would be required if the veneer fails. Here is the typical malpractice scenario: Doc GP provides veneers on heavily prepped teeth after learning the technique at a commercially-driven course. Failure happens. (Debonding and/or sensitivity are the most common.) Patient seeks help from a specialist, often (unfortunately) a prosthodontist (small p or capital "P") who knows little about bonding or veneers. Prosthodontist informs patient that teeth are over-prepped and now require crowns (of course with more tooth reduction, duh!). Something goes wrong, such as now needing endo. Litigation follows now if it did not follow the prosthodontist's initial treatment. On one recent case, it was quite clear to me that the prosthodontist (small p in this case, but you would not know it from his web site) deserved most of the blame. However it was Doc GP who was sued.
Bleaching:
In just about every court case, "bleaching" or "whitening" comes up. If it seems like a reasonable alternative, was the patient informed? Be sure that conversation and especially a rejection is witnessed; have your witness (a DA, perhaps) make a separate chart entry or initial the existing one. If my assistant was not present for the consultation, I make sure she is there for a summary conversation. In my seminars, I am showing some amazing bleach results for tetracycline stained teeth so it could be a reasonable alternative.
Orthodontics:
Orthodontics should include "invisible braces" as part of the informed consent. I was recently asked in court if the "standard of care" should include "Invisalign" in the informed consent. Again, be sure to document well if this treatment option is rejected. This is one which I am personally very, very careful to document.
Speech problems:
I do not generally inform about this one since it is very rare that patients do not adapt. I often tell patients that they can expect some strange feeling teeth for a "few days" but beyond that I am not very concerned. However if you make some radical changes, shall we say "Extreme", it would be a point worth considering in the informed consent.
Crowns to replace:
I simply do not inform as such because it has not, to this day, occurred for me. I have done thousands of veneers, the count is well into five figures. However my veneers are quite conservative; beware if you are a heavy "tooth cutter" using only pressed ceramics, like I see so often in court.
Post-op sensitivity:
Again, a non-problem for me. I think it's because I am so tooth conservative and I believe that I do have a good handle on bonding. I can recall a few teeth that have had some sensitivity, but not more that one in any veneer case. Only once did it not go away within a few days and actually that tooth received endo. The endodontist told me and the patient that it was highly likely the veneer did not cause the problem. BTW, the endodontist stated that a crown after endo would be contraindicated; the veneered tooth would be stronger! Right-on!! (There is a nice reference on this subject; Cumulative effects of successive restorative procedures on anterior crown flexure: intact vs. veneered incisors. Magne P and Douglas W, Quint Inter 2000;31:5-18.)
p.s. I was a witness in a weird case where the patient was completely happy with her veneer shade until about 2 years later, when she changed her mind about the ludicrous white shade she selected. Fortunately it was well documented that she picked the shade and confirmed her good choice later. Then the typical scenario: prosthodontist (small p) makes crowns since allegedly too much tooth was removed (absolutely stupid in this case since enamel remained nearly everywhere). The lesson to be learned here is document and witness so it's not a matter of one dentist against one patient. Juries are sometimes sympathetic and unpredictable but with documentation, less likely to make a bad judgment. BTW, plaintiff's expert stated that veneers are contraindicated on lower incisors, duh. Beware of what you may be up against.
- Veneers are not permanent
- Veneering is irreversible
- Many times bleaching is preferred
- Many times orthodontics (include "invisible braces") is preferred
- Occasional speech problems and food trapping
- Occasionally crowns are required to replace
- Post-op sensitivity can occur
Some of the attorneys I have worked with recommend even more extensive informed consent such as for complications of anesthesia and even tooth loss. I personally think these are so unlikely that I don't generally include them, any more than I would with routine operative dentistry. Of course I'm not an attorney, so you might wish to consult your own attorney about this matter.
Permanent:
Amazingly, a frequent problem that leads to litigation is that patients somehow think veneers are"permanent". Now just what in restorative dentistry is permanent? I can only think of extraction. So let's be sure to inform about expected longevity and especially what happens when they do need replacement. Now think about how advantageous it would be to replace veneers that are entirely in enamel, compared to those placed on heavily prepped teeth, well into dentin. If you don't know the procedure for conservative veneers, may I humbly suggest that you attend my seminar? I also recommend Ross Nash Seminars for such. (If you can't make it to a seminar, one top reference is: Fracture load and mode of failure of ceramic veneers with different preparations. Castelnuevo et al, J Pros Dent 2000;83:171-180).
Irreversible:
DenMat has been advocating "no prep" (reversible) veneers since the 1980's. Lately they seem to have revived the concept with some heavy promotion which has led to increased public and dentist awareness. They seem to have mastered the process of producing very thin veneers. Of course DenMat can work well with prepped teeth too. On most well aligned teeth, I prefer conservative in-enamel preparations for enhanced esthetics and potentially better periodontal response. I tell most of my patients about the advantages I perceive of conservative (in enamel) tooth reduction but of course also the trade-offs compared to "no prep" veneers. My occasional "no-prep" veneers are mostly done on lingually tipped incisors or on peg-shaped lateral incisors. If you do prep, especially heavily and that often means into dentin, be sure that your patients understand. They should be told that occasionally a crown (and perhaps endo too, to be safe) would be required if the veneer fails. Here is the typical malpractice scenario: Doc GP provides veneers on heavily prepped teeth after learning the technique at a commercially-driven course. Failure happens. (Debonding and/or sensitivity are the most common.) Patient seeks help from a specialist, often (unfortunately) a prosthodontist (small p or capital "P") who knows little about bonding or veneers. Prosthodontist informs patient that teeth are over-prepped and now require crowns (of course with more tooth reduction, duh!). Something goes wrong, such as now needing endo. Litigation follows now if it did not follow the prosthodontist's initial treatment. On one recent case, it was quite clear to me that the prosthodontist (small p in this case, but you would not know it from his web site) deserved most of the blame. However it was Doc GP who was sued.
Bleaching:
In just about every court case, "bleaching" or "whitening" comes up. If it seems like a reasonable alternative, was the patient informed? Be sure that conversation and especially a rejection is witnessed; have your witness (a DA, perhaps) make a separate chart entry or initial the existing one. If my assistant was not present for the consultation, I make sure she is there for a summary conversation. In my seminars, I am showing some amazing bleach results for tetracycline stained teeth so it could be a reasonable alternative.
Orthodontics:
Orthodontics should include "invisible braces" as part of the informed consent. I was recently asked in court if the "standard of care" should include "Invisalign" in the informed consent. Again, be sure to document well if this treatment option is rejected. This is one which I am personally very, very careful to document.
Speech problems:
I do not generally inform about this one since it is very rare that patients do not adapt. I often tell patients that they can expect some strange feeling teeth for a "few days" but beyond that I am not very concerned. However if you make some radical changes, shall we say "Extreme", it would be a point worth considering in the informed consent.
Crowns to replace:
I simply do not inform as such because it has not, to this day, occurred for me. I have done thousands of veneers, the count is well into five figures. However my veneers are quite conservative; beware if you are a heavy "tooth cutter" using only pressed ceramics, like I see so often in court.
Post-op sensitivity:
Again, a non-problem for me. I think it's because I am so tooth conservative and I believe that I do have a good handle on bonding. I can recall a few teeth that have had some sensitivity, but not more that one in any veneer case. Only once did it not go away within a few days and actually that tooth received endo. The endodontist told me and the patient that it was highly likely the veneer did not cause the problem. BTW, the endodontist stated that a crown after endo would be contraindicated; the veneered tooth would be stronger! Right-on!! (There is a nice reference on this subject; Cumulative effects of successive restorative procedures on anterior crown flexure: intact vs. veneered incisors. Magne P and Douglas W, Quint Inter 2000;31:5-18.)
p.s. I was a witness in a weird case where the patient was completely happy with her veneer shade until about 2 years later, when she changed her mind about the ludicrous white shade she selected. Fortunately it was well documented that she picked the shade and confirmed her good choice later. Then the typical scenario: prosthodontist (small p) makes crowns since allegedly too much tooth was removed (absolutely stupid in this case since enamel remained nearly everywhere). The lesson to be learned here is document and witness so it's not a matter of one dentist against one patient. Juries are sometimes sympathetic and unpredictable but with documentation, less likely to make a bad judgment. BTW, plaintiff's expert stated that veneers are contraindicated on lower incisors, duh. Beware of what you may be up against.
Smile Design:
The first question is smile design. I try to avoid computer simulations since they can over-promise. What I often do is mock up in the mouth, using either Show Off (Cosmedent) or Estelite Sigma (Tokuyama, my absolute favorite composite). Second, we decide prep, no-prep and if prep, how much. If the tooth length needs to be reduced, just "cut off" the tooth with a black alcohol soluble marker pen as part of the mockup. An example is below:
The first question is smile design. I try to avoid computer simulations since they can over-promise. What I often do is mock up in the mouth, using either Show Off (Cosmedent) or Estelite Sigma (Tokuyama, my absolute favorite composite). Second, we decide prep, no-prep and if prep, how much. If the tooth length needs to be reduced, just "cut off" the tooth with a black alcohol soluble marker pen as part of the mockup. An example is below:
Tooth Preparation:
I tend to follow the "Castelnuevo prep" design, that is plan for 2 mm of incisal free-standing porcelain, a lingual butt joint and a facial reduction of about 1/2 the enamel. (See reference above.) I do not routinely break the contacts.
Impression:
I prefer putty/wash for accuracy and ease of impression. Putty/wash seems to be overlooked by a lot of Americans but it is the most popular in Europe. I specifically do not use "H and H" for veneers since they are not subgingival, where H and H is preferred. I like Danville's Star VPS putty since it does not stick to my gloved fingers. For the wash, I prefer the First Quarter Light or for a big case, the slower Star VPS Light. To prevent tears of the impression where it goes through below the contact, it is helpful to place some of Ultradent's Blue Blockout (ships with Opalescence), to the lingual area and light cure it. The resulting impressions are very clear and free of tears:
I tend to follow the "Castelnuevo prep" design, that is plan for 2 mm of incisal free-standing porcelain, a lingual butt joint and a facial reduction of about 1/2 the enamel. (See reference above.) I do not routinely break the contacts.
Impression:
I prefer putty/wash for accuracy and ease of impression. Putty/wash seems to be overlooked by a lot of Americans but it is the most popular in Europe. I specifically do not use "H and H" for veneers since they are not subgingival, where H and H is preferred. I like Danville's Star VPS putty since it does not stick to my gloved fingers. For the wash, I prefer the First Quarter Light or for a big case, the slower Star VPS Light. To prevent tears of the impression where it goes through below the contact, it is helpful to place some of Ultradent's Blue Blockout (ships with Opalescence), to the lingual area and light cure it. The resulting impressions are very clear and free of tears:
Temporaries:
I etch a small spot in the center of the facial surface, and then apply a light curing enamel bond such as Danville's E-Bond. For one or two veneers, I then hand sculpt some Estelite Sigma composite to the facial surface and light cure it. Thus the composite is spot bonded. For a larger case, I use TurboTemp 2 or Luxatemp (Turbo-Temp 2 is a far better value) in a preliminary impression. The preliminary impression is made after mocking up the teeth so that the proposed changes are in the temps. After the TurboTemp 2 is self cured in the mouth for about two minutes, I remove the impression and light cure the E-Bond through the TurboTemp 2. It attaches to the previously light cured E-Bond.
Try-in:
For try-in, silane (such as S-Bond) is placed on the HF lab etched veneers while they are clean. Now there are two recommended procedures. For years I have used Danville's E-Bond on the veneer to protect the silane from contamination. First, I try-in for fit with the silane and E-Bond on the veneers. Then I add composite (currently, Accolade PV Try-in composite, see below) to the E-Bond and try in for color. The E-Bond is light sensitive so it has some effect on limiting the try-in time. The second procedure, a great innovation from Danville, uses Accolade PV Try-in Composite placed directly on the silane, no E-Bond. The veneer is tried in for fit and color simultaneously. Accolade PV Try-in is real composite but has no light sensitive initiators, thus allowing accurate color evaluation with nearly unlimited try-in time. Using a composite rather than a glycerine based try-in materials not only speeds the procedure but also eliminates the possibility of contamination by the try-in material. After try-in, the trick is to remove at least 50% of the Accolade PV Try-in composite and then replace it with the normal catalyzed Accolade PV composite. The remnant Try-in material is polymerized by what's known as "diffusion polymerization". This technique is unique in the industry and I very highly recommend it. Danville supplies complete technique instructions with the Accolade PV kit. For further efficiency of try-in, I try-in with two shades of composite simultaneously as illustrated below. By observing the two shades, I can "dial in" a composite blend if required or just choose the best shade. If there is more than one veneer, I usually try-in with different shades on each veneer. Sometimes just a "right half" and a "left half" on a big case. The unlimited try-in time allows the patient to take as much time as required for try-in and I proceed only when they are happy with the shade. No more remakes on me! As my good friend, Dr. Tom Hughes of Colorado says, the patient "buys the shade" before the veneers are bonded. They can take as much time as they want.
I etch a small spot in the center of the facial surface, and then apply a light curing enamel bond such as Danville's E-Bond. For one or two veneers, I then hand sculpt some Estelite Sigma composite to the facial surface and light cure it. Thus the composite is spot bonded. For a larger case, I use TurboTemp 2 or Luxatemp (Turbo-Temp 2 is a far better value) in a preliminary impression. The preliminary impression is made after mocking up the teeth so that the proposed changes are in the temps. After the TurboTemp 2 is self cured in the mouth for about two minutes, I remove the impression and light cure the E-Bond through the TurboTemp 2. It attaches to the previously light cured E-Bond.
Try-in:
For try-in, silane (such as S-Bond) is placed on the HF lab etched veneers while they are clean. Now there are two recommended procedures. For years I have used Danville's E-Bond on the veneer to protect the silane from contamination. First, I try-in for fit with the silane and E-Bond on the veneers. Then I add composite (currently, Accolade PV Try-in composite, see below) to the E-Bond and try in for color. The E-Bond is light sensitive so it has some effect on limiting the try-in time. The second procedure, a great innovation from Danville, uses Accolade PV Try-in Composite placed directly on the silane, no E-Bond. The veneer is tried in for fit and color simultaneously. Accolade PV Try-in is real composite but has no light sensitive initiators, thus allowing accurate color evaluation with nearly unlimited try-in time. Using a composite rather than a glycerine based try-in materials not only speeds the procedure but also eliminates the possibility of contamination by the try-in material. After try-in, the trick is to remove at least 50% of the Accolade PV Try-in composite and then replace it with the normal catalyzed Accolade PV composite. The remnant Try-in material is polymerized by what's known as "diffusion polymerization". This technique is unique in the industry and I very highly recommend it. Danville supplies complete technique instructions with the Accolade PV kit. For further efficiency of try-in, I try-in with two shades of composite simultaneously as illustrated below. By observing the two shades, I can "dial in" a composite blend if required or just choose the best shade. If there is more than one veneer, I usually try-in with different shades on each veneer. Sometimes just a "right half" and a "left half" on a big case. The unlimited try-in time allows the patient to take as much time as required for try-in and I proceed only when they are happy with the shade. No more remakes on me! As my good friend, Dr. Tom Hughes of Colorado says, the patient "buys the shade" before the veneers are bonded. They can take as much time as they want.
Bonding the veneers:
After try-in is satisfactory and patient "buys the shade", the veneers with Try-in Accolade PV composite are removed from the teeth. The teeth are pumiced with a prophy cup to remove all try-in materials from the teeth. The veneers are brushed with Prelude adhesive #2 (included in Accolade PV kits), to dissolve most of the Try-in composite. Then regular Accolade PV is placed on the veneers, not completely rid of Try-in material. These materials are light sensitive so protect from light. Etch the teeth with phosphoric acid (the self etching primer, Prelude #1, is not used) and place the Prelude #2 adhesive on the teeth and then place the veneers. Light cure as usual. As many of you know, I like Clearfil Photo Bond on teeth in situations where complete light cure is doubtful. Photo Bond is dual cured and will perform well even if not light cured. So Photo Bond would be a wise choice for opaque or thick veneers while Prelude is fine for light curable veneers.
After try-in is satisfactory and patient "buys the shade", the veneers with Try-in Accolade PV composite are removed from the teeth. The teeth are pumiced with a prophy cup to remove all try-in materials from the teeth. The veneers are brushed with Prelude adhesive #2 (included in Accolade PV kits), to dissolve most of the Try-in composite. Then regular Accolade PV is placed on the veneers, not completely rid of Try-in material. These materials are light sensitive so protect from light. Etch the teeth with phosphoric acid (the self etching primer, Prelude #1, is not used) and place the Prelude #2 adhesive on the teeth and then place the veneers. Light cure as usual. As many of you know, I like Clearfil Photo Bond on teeth in situations where complete light cure is doubtful. Photo Bond is dual cured and will perform well even if not light cured. So Photo Bond would be a wise choice for opaque or thick veneers while Prelude is fine for light curable veneers.
Clearfil Ceramic Primer (Kuraray)
One of the most confusing current issues is how to bond to various ceramic materials. We all know how to bond to "silica" based, HF etched porcelain, by using silane. Many of you know my favorite silane product, Clearfil Porcelain Bond Activator, which eliminates the need for the HF etching step on silica based porcelain. This is a unique property of Activator, no HF required. (Ref: Fatigue span of porcelain repair systems. Llobell A et al, Int J Pros 1992;5:205-213.) Activator is not used by itself, it is mixed with an appropriate Clearfil primer. However if the ceramic is not made of silica and therefore not HF-etchable [examples Lava (3M/Espe) and Procera (Nobel)] silane does not work and Activator does not work either. Matter of fact, any and all silanes act like a separator! So I have recommended sandblast with aluminum oxide followed by either Panavia or Bistite. This method for bonding is confirmed by the research of Prof. Mathias Kern in Germany. An alternative, although more trouble and more expensive but certainly working well, is to use Rocatec or CoJet (3M/Espe). All of this has proven to be very confusing. Kuraray has solved the confusion (or perhaps introduced more) by combining two technologies, the silane properties of Clearfil Porcelain Bond Activator and the adhesion monomer of Panavia. The product is called Clearfil Ceramic Primer which bonds to just about any ceramic (silica or non-silica based), no HF etching required. "If it's white, just sandblast and use Clearfil Ceramic Primer; it will bond". The Ceramic Primer will link to just about any composite luting cement such as Variolink 2 (Vivadent) or Kuraray's new Esthetic Cement. Of course Ceramic Primer also works with Panavia but it is redundant for non-etchable ceramics. Now at the risk of confusion, Ceramic Primer works on non-precious metals too. If this is all overwhelming, consider attending my seminar. We will clear up any confusion. I will give you a cookbook procedure. Since Clearfil Ceramic Primer is a brand new product, it might not yet be on the dealer shelves. I bet that Tin Man will be among the first to stock it: (800) 554-6394.
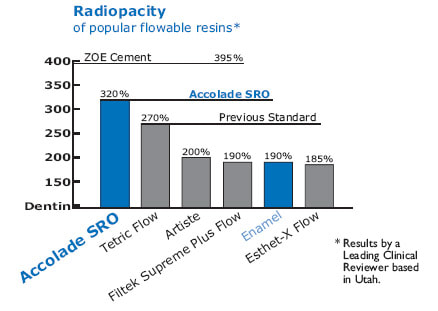
Accolade SRO (Danville)
Two of the best selling flowable composites in the USA are StarFlow and "high viscosity StarFlow" known as Accolade. StarFlow had the highest compressive strength of all flowable composites in CRA testing. It was found to be stronger than some "packable" composites. StarFlow and Accolade compare to Herculite in strength yet both are flowable composites! Now there is a new version, Accolade SRO, meaning "Super RadiOpaque". SRO has the highest radiopacity of any known composite, making it ideal as a first increment for posterior composites. Now highest strength and highest radiopacity have been combined. The SRO is not quite as esthetic as the regular Vita shades of StarFlow so it is recommended for first increments only.
What Determines the Wear Rate of Composites?
I keep seeing higher and higher filler contents of composite advertised. I presume that a lot of docs would equate this higher filler content with lower wear rate. This conclusion is most likely incorrect. Filler size has a greater influence on wear rate than does percent filler. A great example is Vivadent's HelioMolar. That material clearly outperforms all other composites for wear resistance (and stays polished too) yet it has a very low percentage fill. The reason is simple: the small particle size of the "microfill" filler. Please note that while HelioMolar is a superb choice as a final increment, it may be less that ideal for the bulk of the filling since it is relatively weak. So for years I have recommended that a hybrid composite be used underneath the final layer of HelioMolar. Personally, I use the flowable hybrid StarFlow as a "base". These days I bond it with Danville's Prelude SE.
Ray's Current Recommendations:
Class I, II, and V composites
Class III and IV Composites
Bonded Amalgam
Indirect restorations that require dual-curing (eg. crowns)
Indirect restorations that are light curable (eg. veneers)
Bases
Bonding to existing porcelain or composite
Bonding to existing metal
- Prelude SE Bond
- Clearfil SE Bond
Class III and IV Composites
- Total etch and Clearfil Photo Bond
- Total etch and Prelude #2
Bonded Amalgam
- Total etch, Microprime G, Clearfil Photo Bond
Indirect restorations that require dual-curing (eg. crowns)
- Panavia F 2.0 (Normal set: ED Primer; Slow set: total etch, Photo Bond)
- Prelude SE with Link, then dual cure composite such as Starfill 2B
- Variolink 2
Indirect restorations that are light curable (eg. veneers)
- Total etch, Prelude #2
- Clearfil Photo Bond and Accolade PV
Bases
- Fiji VII, only if residual caries, otherwise no base
Bonding to existing porcelain or composite
- Sandblasting followed by Clearfil Photo Bond mixed with Porcelain Bond Activators
Bonding to existing metal
- Sandblasting followed by Panavia F 2.0 (tin-plate after sandblasting if precious metal, OR use Tokuyama Metaltite if not tin-plated)